Hepatomegaly: What It Really Means Through a Genomics + Functional Medicine Lens

“We don’t chase symptoms — we rebuild systems.”
INTRODUCTION — When the Liver Speaks, It Speaks Early
Dr. Wellman, a retired school teacher in his early sixties, never thought much about his liver. It wasn't until a routine check-up revealed an enlarged liver that he started to wonder about his health. This seemingly silent message from one of the body's most crucial organs signaled a change that would lead him on a transformative health journey. Hepatomegaly, while not a diagnosis, was his body's way of alerting him to the shifts happening beneath the surface.
Traditional medicine provides the essential framework for identifying hepatomegaly and ruling out serious structural or pathological conditions. Functional medicine and genomics then explore the metabolic, inflammatory, and genetic patterns that influence liver behavior, prompting a deeper question:
“What is pushing the liver to work harder — and what does that reveal about the system/code beneath the symptom?”
Because hepatomegaly is rarely random.
It’s a downstream expression of upstream biology, including detoxification capacity, genetics, inflammation, hormones, body composition, infections, and even micronutrient status. For example, a nightly glass of wine coupled with low choline genes can exacerbate liver enlargement, illustrating how daily choices interact with our genetic predispositions.
This article breaks it down in the language of systems — not symptoms.
SECTION 1 — The Liver: The Body’s Metabolic Command Center
The liver manages over 500 functions every single day:
- Detoxification (Phase I, II, III pathways)
- Hormone metabolism
- Methylation + epigenetic regulation
- Lipid transport + cholesterol balancing
- Glycogen storage
- Bile production
- Immune surveillance
- Antioxidant cycling (glutathione system)
When the liver enlarges, one of two things is happening:
✅ 1. Increased workload (adaptive hypertrophy/enlargement)
The liver is trying to keep up with a demand that exceeds its baseline:
- High toxic load
- Medications
- Alcohol
- Environmental exposures
- Chronic inflammation
- Fat accumulation
- Microbial endotoxin burden
- Biliary congestion (gallbladder dysfunction)
- Pancreatic inflammation is blocking biliary flow
- Portal pressure changes from spleen or gut inflammation
✅ 2. Structural or inflammatory changes
Fibrosis, congestion, infiltration, infections, or immune dysregulation.
In both scenarios, hepatomegaly is a warning — a metabolic overload alert.
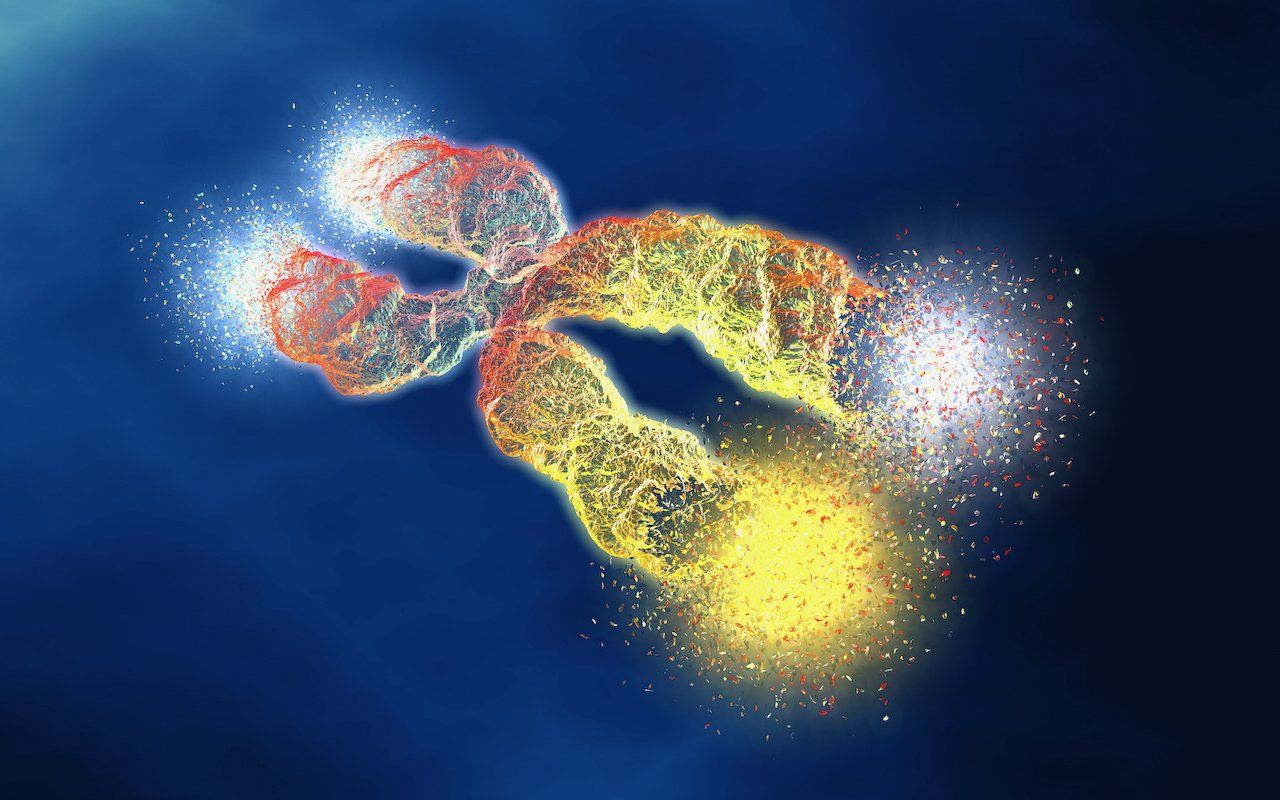
SECTION 2 — The Genomics Perspective: Your Liver's Operating System
Genetic variations determine how efficiently your liver can detox, process hormones, and neutralize oxidative stress. Although these SNPs do not cause hepatomegaly by themselves, they define your vulnerability when lifestyle, diet, or toxicity exceeds capacity. However, just as software can be updated, these genetic predispositions can often be influenced by our choices, highlighting that they are not immutable destinies but modifiable codes.
Key Genomic Pathways Linked to Hepatomegaly
1. Phase I Detox (Cytochrome P450 enzymes)
These convert fat-soluble toxins into reactive intermediates.
- CYP1A2 – caffeine + toxins
- CYP3A4 – medications, steroids, alcohol
- CYP2E1 – alcohol, solvents, industrial chemicals
Fast Phase I and Slow Phase II lead to liver stress and inflammation. So what does this mean in real-world terms? When these detoxification phases are out of balance, substances like acetaminophen can linger in the body up to three times longer, increasing the risk of inflamed tissue and liver damage.
2. Phase II Detox (Conjugation Pathways)
These neutralize and eliminate toxic intermediates:
- GSTM1 / GSTT1 deletion → lower glutathione capacity
- GSTP1 variants → increased oxidative stress
- COMT V158M → slower estrogen + catecholamine clearance
- UGT1A1*28 → bilirubin challenges
- SULT1A1 variants → impaired hormone metabolism
When Phase II lags, toxic intermediates accumulate → hepatocyte stress → enlargement.
3. Methylation System (MTHFR, MTR, BHMT)
Poor methylation increases:
- Homocysteine
- Oxidative stress
- Estrogen metabolite buildup
- Impaired repair of hepatocytes
This slows liver regeneration — a key factor in reversing hepatomegaly.
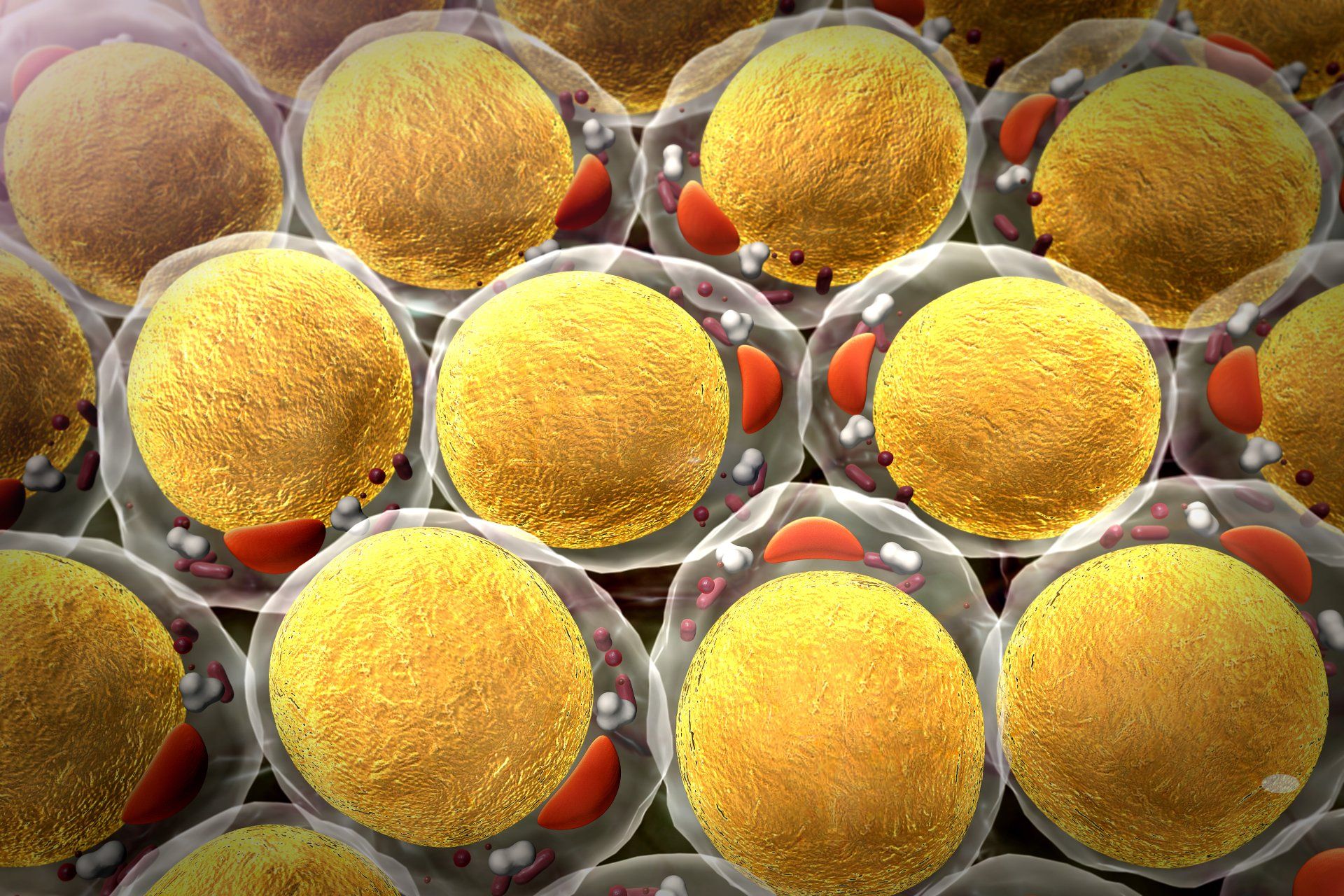
4. PNPLA3 + TM6SF2 (Fat Accumulation Genes)
These determine your risk for:
- Fatty liver
- Steatohepatitis
- Hepatic inflammation
Carriers of PNPLA3 rs738409 G allele can develop enlargement even with “normal” lifestyle habits.
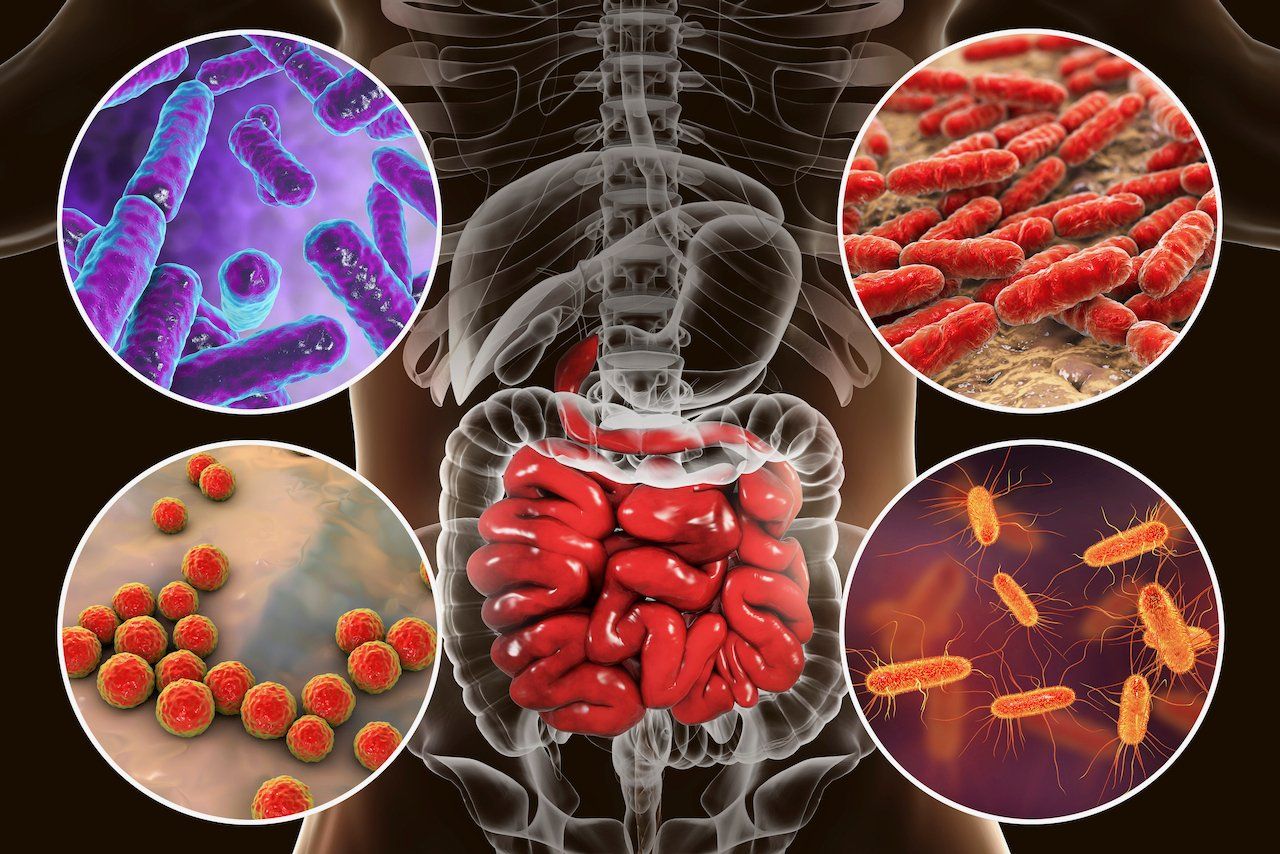
5. NOD2 + TLR4 (Microbial + Endotoxin Sensitivity)
Heightened response to gut-derived endotoxins → portal inflammation → hepatomegaly.
This is why gut issues and liver enlargement are often inseparable.
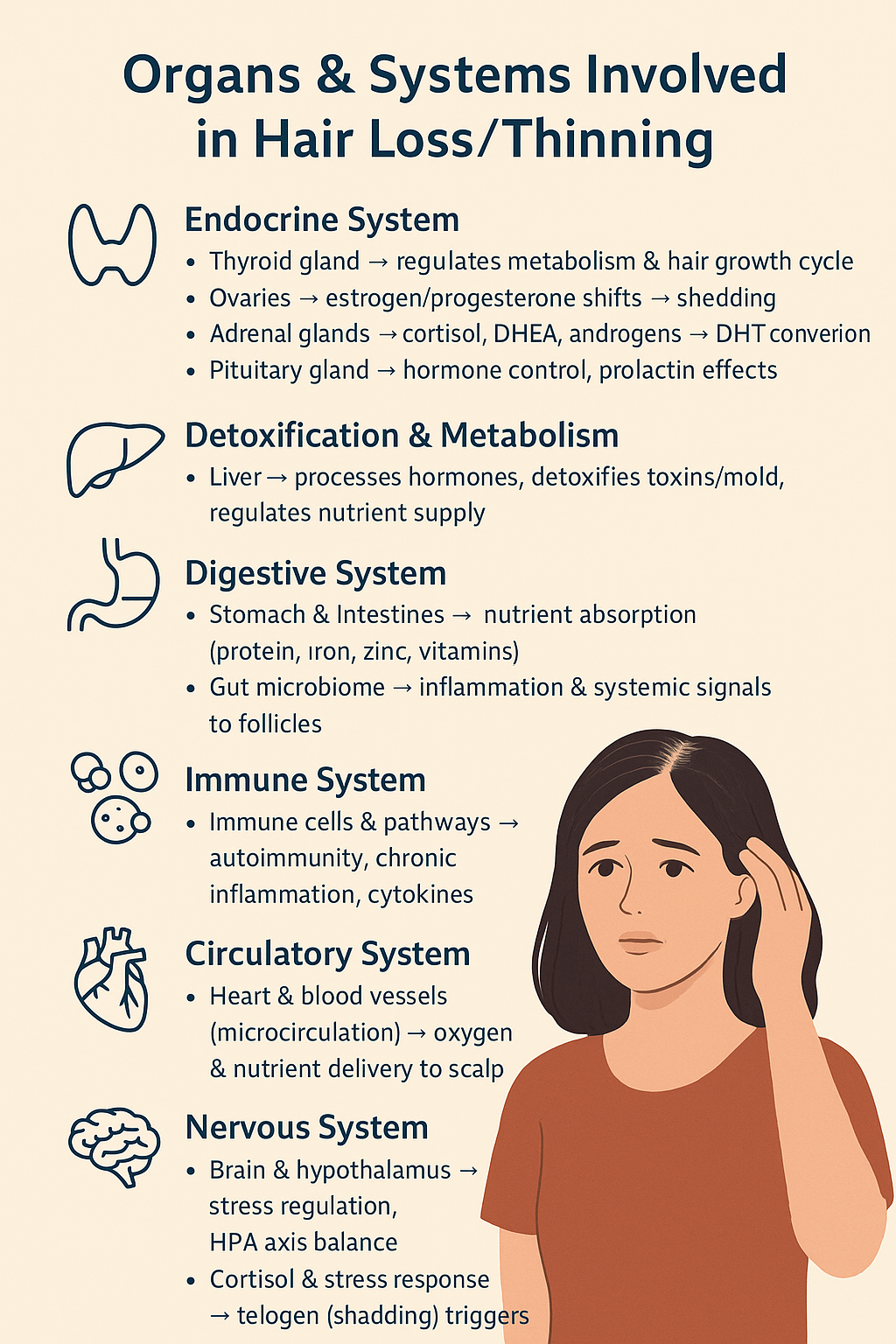
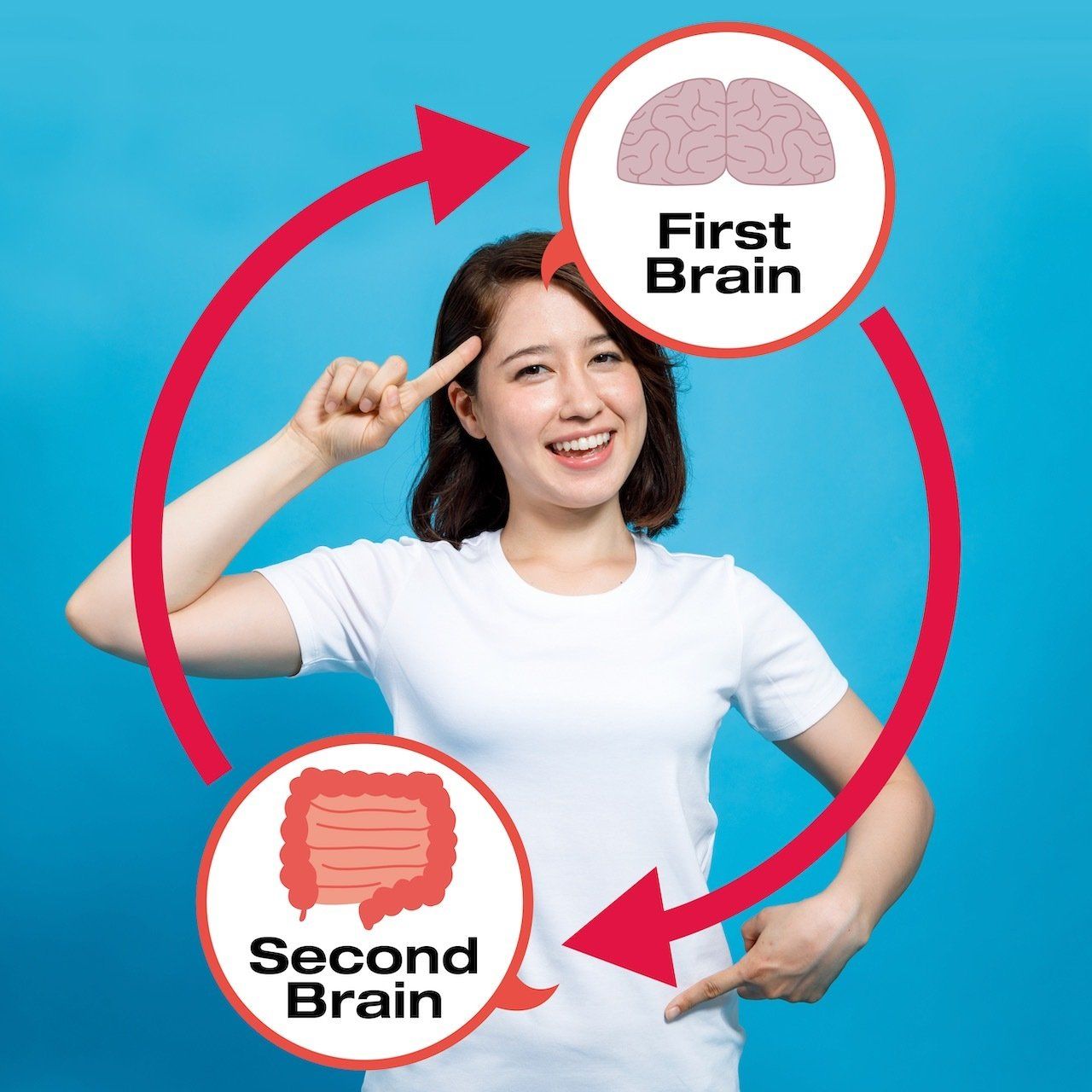
SECTION 3 — Functional Medicine View: The 8 Systems and How They Feed the Liver
In the Michael DC systems model, hepatomegaly reflects an imbalance in at least one of the 8 functional systems, often more than one. Consider the case of Jane, a 45-year-old nurse. She experienced symptoms like bloating and fatigue, which prompted her to seek medical advice. Upon analysis, it became evident that her gut-liver axis and hormone system were imbalanced. Jane's diet was heavily laden with refined carbohydrates and lacked fiber, contributing to her gut dysbiosis and endotoxin exposure. Simultaneously, stress and environmental factors were exacerbating her estrogen dominance due to slow COMT function. By adjusting her diet to include more fiber-rich foods, reducing her sugar intake, and implementing stress-reduction techniques, Jane managed to alleviate her symptoms. Additionally, her treatment plan included supplements to support COMT function, such as magnesium and B vitamins, which further helped improve her hormonal balance and liver health.
✅ 1. Gastrointestinal System
The GI tract has the most direct impact on the liver through the gut–liver axis.
- Dysbiosis
- SIBO
- H. pylori
- Leaky gut
- Endotoxin load
- IBS (gas pressure, motility issues → toxin recirculation)
- IBD (Crohn’s/UC → cytokine spillover → hepatic inflammation)
- Duodenitis/gastritis → impaired bile flow → hepatic congestion
These increase hepatic inflammation through the portal vein.
✅ 2. Detoxification System
- Poor Phase I/II balance
- Low glutathione
- Nutrient deficiencies
- Medication overload
The liver swells when detox demand exceeds its detox capacity. To illustrate the importance of detox balance, studies have shown that in patients with NAFLD, there is often a 70% depletion of glutathione, a critical antioxidant that helps protect liver cells from damage.
✅ 3. Hormone System
Estrogen dominance, androgen therapy, thyroid dysregulation — all can enlarge the liver through inflammatory and metabolic shifts.
✅ 4. Immune + Inflammatory System
Low-grade chronic inflammation increases hepatic macrophage activation (Kupffer cells) → liver enlargement.
✅ 5. Metabolic System
- Insulin resistance
- Obesity
- Fatty liver
- Pancreatic fat/pancreatitis → bile duct obstruction → hepatic swelling
These are the number one causes of hepatomegaly in the modern world. By using digital health tools such as continuous glucose monitors, individuals can gain real-time insights into their insulin resistance, enabling personalized interventions aligned with metabolic health data. This technology empowers users to track and understand how different lifestyle choices directly impact their liver health, further refining the narrative of functional medicine in a digital age.
✅ 6. Nutrient System
Low levels of:
- Choline
- Folate
- B12
- NAC
- Glycine
- Vitamins A/D/E/K
- Omega-3
Directly impair liver repair + detox pathways.
✅ 7. Structural System
- Visceral fat compressing the liver
- Gallbladder restriction or ductal obstruction
- Pancreatic inflammation is blocking the biliary tree
- Spleen enlargement increases portal pressure
✅ 8. Circulatory System
- Congestive changes (from right-sided heart issues)
- Portal hypertension
- Splenic backup
It can enlarge the liver due to increased pressure.
SECTION 4 — The 5 Most Common Functional Causes of Hepatomegaly
1. Non-alcoholic fatty liver (NAFLD) — metabolic + genetic
Driven by insulin resistance + PNPLA3/TM6SF2 variants.
2. Estrogen overload
Slow COMT + low methylation → estrogen metabolites accumulate → hepatic congestion.
3. Gut-liver axis dysfunction
Endotoxin exposure from dysbiosis, IBS, IBD, SIBO, gastritis, H. pylori → hepatic inflammation.
4. Toxin burden + slow detox genetics
Environmental chemicals, medications, molds, solvents, and alcohol.
5. Micronutrient depletion
Choline, omega-3, folate, B12, antioxidants.
SECTION 5 — Typical Symptoms Patients Notice
Not everyone feels symptoms, but common ones include:
- Right upper quadrant fullness
- Bloating after meals
- Early satiety
- Distension
- Intermittent discomfort
- Fatigue after eating
- Poor alcohol tolerance
- Brain fog
- High sensitivity to supplements/meds
- Pain or pressure worsened by fatty meals (gallbladder)
- Pain radiating to the back (pancreatitis)
- IBS flares are worsening RUQ pressure
- IBD-related fatigue and inflammation burden
These correlate strongly with detox + inflammation overload.
✅ INTERWOVEN NEW SECTION — How Other Organs Influence Hepatomegaly
Gallbladder
- Sluggish bile → hepatic congestion
- Gallstones → obstruction
- Biliary dyskinesia → poor bile release
- Post-cholecystectomy → increased hepatic workload
Key genetics: ABCB11, ABCC2, PEMT.
Pancreas
- Pancreatitis blocks the common bile duct → liver swelling
- Fatty pancreas mirrors fatty liver
- Shared metabolic pathways (PNPLA3)
Stomach + Duodenum
- Gastritis
- Duodenitis
- H. pylori
All → cytokine spillover + impaired bile flow → hepatic congestion.
Small Intestine: IBS + SIBO
- IBS → motility issues → toxic recirculation
- SIBO → endotoxin overload → portal inflammation
Large Intestine: IBD + IBS
- IBD → systemic inflammation → hepatic swelling
- IBS-C → toxin reabsorption
- IBS-D → bile acid dysregulation
Spleen
- Splenomegaly increases portal pressure → hepatic engorgement.
Cardiovascular
- Right-sided heart dysfunction → hepatic congestion.
Lymphatics
- Stagnant lymph flow → slowed hepatic drainage.
Endocrine
- Estrogen, thyroid, cortisol, testosterone → all influence liver size.
SECTION 6 — Advanced Functional Testing
✅ Tier 1 (Immediate Panels)
- Liver enzymes
- Bilirubin
- GGT
- Lipid panel
- Fasting glucose + Insulin + HOMA-IR
- Ferritin
- CRP/ESR
- Viral hepatitis screen
- Amylase, lipase (pancreas)
- Bilirubin fractionation (biliary issues)
✅ Tier 2 (Expansion)
- Hormone panel (Estrogen metabolites + cortisol)
- Comprehensive stool test
- SIBO breath test
- ANA + autoimmune markers
- GB ultrasound (gold standard -sludge, stones, EF)
- Pancreas imaging, if indicated
✅ Tier 3 (Genomics + Deep Systems)
- Liver detox panel (CYP, GST, SULT, COMT, UGT)
- PNPLA3/TM6SF2
- MTHFR + methylation
- Choline metabolism genes (PEMT)
- Gut immune SNPs (NOD2, TLR4)
- ABCB11 (bile transport)
- SPINK1/CTRC/PRSS1 (pancreatitis genetics)
This is where functional medicine shines. We rebuild the system with a personalized approach, recognizing that each patient’s needs may vary. When implementing the protocol, careful consideration is given to customize it for patients with comorbidities or those on multiple medications. This ensures that the care provided is both safe and individualized.
This is where functional medicine shines — we rebuild the system.
PHASE 1 — Reduce Inflammatory Load (2–4 weeks)
- Anti-inflammatory diet
- Remove alcohol, sugar, and seed oils
- Lower endotoxin exposure
- Begin NAC + glycine + B-complex
- Magnesium glycinate
- Omega-3
- Light movement daily
- Hydration + electrolytes
- Soften bile (dandelion, bitters, taurine, choline)
- Support the pancreas if it is inflamed (enzymes, low-fat meals)
- Reduce IBS/IBD triggers
PHASE 2 — Optimize Detox Pathways (4–8 weeks)
- Glutathione support
- Bile flow support (TUDCA, milk thistle, dandelion, bitters)
- Support Phase II (methylation, sulfation, glucuronidation)
- Increase cruciferous vegetables
- Add choline (eggs or phosphatidylcholine)
- Gallbladder support + biliary drainage
- SIBO protocol if positive
PHASE 3 — Repair, Regenerate, Rebuild (8–12+ weeks)
- Address gut dysbiosis
- Heal intestinal permeability
- Complete hormone balancing
- Correct micronutrients
- Restore mitochondrial function
- Reassess liver size
- Pancreas recovery if involved
- IBD inflammation management
The liver regenerates rapidly when the inputs and the genetic pathways are aligned. It is famously known for its ability to regenerate up to 30% of its mass within just eight weeks. This phenomenal capacity offers tremendous hope for recovery, reinforcing the idea that, with the right interventions, full liver health is achievable.
SECTION 8 — When to Worry
Seek escalation if you see:
- Jaundice
- Persistent RUQ pain
- Fever
- Vomiting
- Unintentional weight loss
- Severe fatigue
- Elevated liver enzymes (ALT > 100, AST > 100)
- Very high ferritin
- Worsening bilirubin
- Severe epigastric pain radiating to the back (pancreatitis)
- Dark urine + pale stools (biliary obstruction)
CONCLUSION - The Liver Doesn't Fail Overnight
Hepatomegaly is one of the earliest signs the body gives when systems begin to drift out of sync. Functional medicine doesn’t silence that signal. It decodes it and rebuilds the metabolic environment that caused it. Hepatomegaly is not a life sentence. It’s a window of opportunity. With the right genomic insights, nutrient strategy, detoxification optimization, and lifestyle design, the liver can fully regenerate—often faster than patients expect. Because biology isn’t fixed. It’s programmable.
To transform insight into practice, I invite you to choose one upstream lever to adjust this week. Whether it's tweaking your diet, incorporating a new supplement, or simply being more mindful of your daily habits, this small change can set you on the path to improved liver health and overall well-being.
Your health isn’t random. It’s written in code. Every cell in your body carries a script. Your genes don’t just predict your future—they respond to what you eat, how you move, and the choices you make daily. That’s the journey I share in “Understanding Genomics: How Nutrition, Supplements, and Lifestyle Can Help You Unlock Your Genetic Superpowers”.
Read the code. Live the design. The rest follows.
Dr. Marios Michael
✅ DISCLAIMER
This content is for informational and educational purposes only.
It is not intended to provide medical advice, diagnose conditions, treat any disease, or replace individualized guidance from your licensed healthcare provider.
The information presented here reflects general functional medicine and genomics concepts and should not be used as a substitute for medical evaluation, especially in the presence of symptoms such as abdominal pain, jaundice, unexplained weight loss, fever, vomiting, or abnormal liver function test results.
Dr. Marios Michael, cFMP, CNS, cFMP, DAAPM, DC, MUA is a Chiropractic Physician and Functional Medicine Practitioner.
Chiropractic physicians do not diagnose or treat medical conditions outside the chiropractic scope of practice. Any discussion of laboratory findings, liver conditions, hepatomegaly, gastrointestinal disorders, or systemic physiology is for educational interpretation only and is not intended to provide medical management of these conditions.
Statements regarding supplements have not been evaluated by the Food and Drug Administration. Products mentioned are not intended to diagnose, treat, cure, or prevent any disease.
Always consult your primary care physician, gastroenterologist, hepatologist, or other licensed medical doctor before making changes to your diet, medications, supplements, or health regimen—especially if you have known liver, gallbladder, pancreatic, gastrointestinal, or metabolic conditions.
Reading this article does not create a doctor–patient relationship with Dr. Michael or Michael DC, and no personalized health advice is being given.
If you believe you are experiencing a medical emergency, call 911 or seek immediate medical care.
REFERENCES (PubMed/PMC)
Liver physiology & regeneration
- Michalopoulos GK. Liver regeneration. J Cell Physiol. 2007;213(2):286-300. PubMed
- Michalopoulos GK. Liver regeneration: biological and pathological mechanisms. Nat Rev Gastroenterol Hepatol.2021;18:40-55. PubMed
Cytochrome P450 / Phase I detox
3) Nebert DW, Russell DW. Clinical importance of the cytochromes P450. Lancet. 2002;360:1155-62. PubMed
Phase II conjugation (UGT, SULT, GST) & bilirubin transport
4) Gamage N, et al. Human sulfotransferases and their role in chemical metabolism. Toxicol Sci. 2006;90(1):5-22. PubMed+1
5) Hayes JD, Strange RC. Glutathione S-transferase polymorphisms and their biological consequences. Pharmacol Ther.2000;85(2):135-70. PubMed
6) Oda S, et al. Function, genetic polymorphism, and regulation of UGT1A1. Drug Metab Pharmacokinet. 2013;28:206-18. PubMed
7) Dean L. UGT1A1 and bilirubin (CPIC/PharmGKB resources). Pharmacogenet Genomics. (overview) PMC+1
8) Mao YX, et al. Transport mechanism of human bilirubin transporter ABCC2/MRP2. Nat Commun. 2024;15:3161. PMC
9) Keppler D. Roles of MRP2, MRP3, OATP1B1/1B3 in bilirubin handling. Pflugers Arch. 2014;466:611-28. PubMed
Bile formation & biliary transporters (gallbladder/bile flow)
10) Lam P, et al. BSEP/ABCB11 in bile salt secretion—clinical aspects. Semin Liver Dis. 2010;30:125-33. PubMed
11) Hayashi H, Sugiyama Y. BSEP/ABCB11 trafficking and cholestasis. Hepatol Res. 2013;43:132-48. PubMed
12) Stieger B. BSEP impairment and cholestatic disease (review). Biochim Biophys Acta. 2011;1812:1238-46. PubMed
Hepatic fat genetics (PNPLA3, TM6SF2)
13) Romeo S, et al. PNPLA3 variant confers susceptibility to NAFLD. Nat Genet. 2008;40(12):1461-5. PubMed+1
14) Kozlitina J, et al. TM6SF2 variant affects hepatic triglycerides/VLDL secretion. Nat Genet. 2014;46:352-6. PubMed
Gut–liver axis, SIBO, H. pylori, IBD
15) Augustyn M, et al. SIBO and NAFLD—mechanisms/evidence. Clin Exp Hepatol. 2019;5(3):183-90. PMC
16) Gudan A, et al. Association between SIBO and NAFLD (review). World J Hepatol. 2023;15:705-22. PMC
17) Mantovani A, et al. H. pylori and risk of MASLD/NAFLD (meta-analysis). Liver Int. 2024. PubMed
18) Okushin K, et al. H. pylori infection and liver diseases (review). World J Gastroenterol. 2018;24:3617-25. PMC
19) Fousekis FS, et al. Hepatobiliary manifestations in IBD. Ann Gastroenterol. 2018;31:274-84. PubMed
20) Gaspar R, et al. Liver manifestations and complications in IBD. World J Hepatol. 2021;13:1709-26. PubMed
Pancreas/pancreatitis genetics and biliary–pancreatic interplay
21) LaRusch J, Whitcomb DC. Genetics of pancreatitis (PRSS1, SPINK1, CFTR, CTRC). Curr Opin Gastroenterol.2011;27:467-74. PubMed
22) GeneReviews: PRSS1-related hereditary pancreatitis. NCBI Bookshelf. 2012-update. NCBI
23) Panchoo AV, et al. Hereditary pancreatitis—updated review. World J Clin Pediatr. 2022;11:33-49. PubMed
Portal circulation, spleen/portal pressure, cardio-hepatic
24) Bloom S, et al. Portal hypertension: pathophysiology, diagnosis, management. BMJ. 2015;351:h4597. PubMed
25) Guixé-Muntet S, et al. Pathophysiology & therapy of cirrhotic portal hypertension (update). Nat Rev Gastroenterol Hepatol. 2024;21:238-56. PubMed
26) Xanthopoulos A, et al. Heart failure & liver disease—cardiohepatic interactions. JACC Heart Fail. 2019;7:87-97. PubMed+1
27) Haddadin R, et al. Congestive hepatopathy—review. Cureus. 2024;16:e60264. PMC
Hepatic lymphatics & immune activation (Kupffer/TLR4)
28) Ohtani O, Ohtani Y. Lymph circulation in the liver. Anat Rec (Hoboken). 2008;291:643-52. PubMed
29) Jeong J, et al. Hepatic lymphatic vascular system in health & disease. J Hepatol. 2022;76:1109-23. PMC
30) Rivera CA, et al. TLR4-dependent Kupffer cell activation in liver injury. Am J Physiol Gastrointest Liver Physiol.2007;293:G1134-42. PMC
31) Guo J, et al. TLR4 in liver injury and fibrogenesis. Front Biosci. 2010;2:1356-66. PMC
Nutrients/methylation/choline/glutathione relevant to detox & repair
32) Corbin KD, Zeisel SH. Choline metabolism & NAFLD insights. Curr Opin Gastroenterol. 2012;28:159-65. PubMed+1
33) Spencer MD, et al. Choline deficiency, microbiome & fatty liver in humans. Gastroenterology. 2011;140:976-86. PubMed+1
34) Zeisel SH. Dietary choline deficiency and genomic/mitochondrial effects. Mutat Res. 2012;733:34-42. PubMed
35) Lu SC. Glutathione synthesis—regulation & liver disease. Biochim Biophys Acta. 2013;1830:3143-53. PubMed
36) Vairetti M, et al. Changes in hepatic glutathione in liver diseases (update). Antioxidants (Basel). 2021;10:364. PMC
37) Raghubeer S, Matsha TE. MTHFR C677T in one-carbon metabolism & epigenetics. Nutrients. 2021;13:3186. PMC+1
Omega-3 / NAFLD (optional dietary support evidence)
38) Aziz T, et al. Omega-3 PUFA efficacy in NAFLD (systematic review/meta-analysis). Nutr Rev. 2024;82:156-170. PubMed
39) Sangouni AA, et al. Omega-3 supplementation and fatty liver indices. Clin Nutr ESPEN. 2021;44:484-490. PubMed
Choline/PEMT genetics & NAFLD risk
40) Piras IS, et al. Hepatic PEMT expression decreases with NAFLD severity; PEMT variants linked to risk. Hepatol Commun. 2022;6:2684-2699. PMC
41) Song J, et al. PEMT polymorphism (V175M) and susceptibility to NAFLD. Hum Mol Genet. 2005;14:1249-56. PMC