When Your Hair Speaks: What Female Hair Loss Really Tells Us
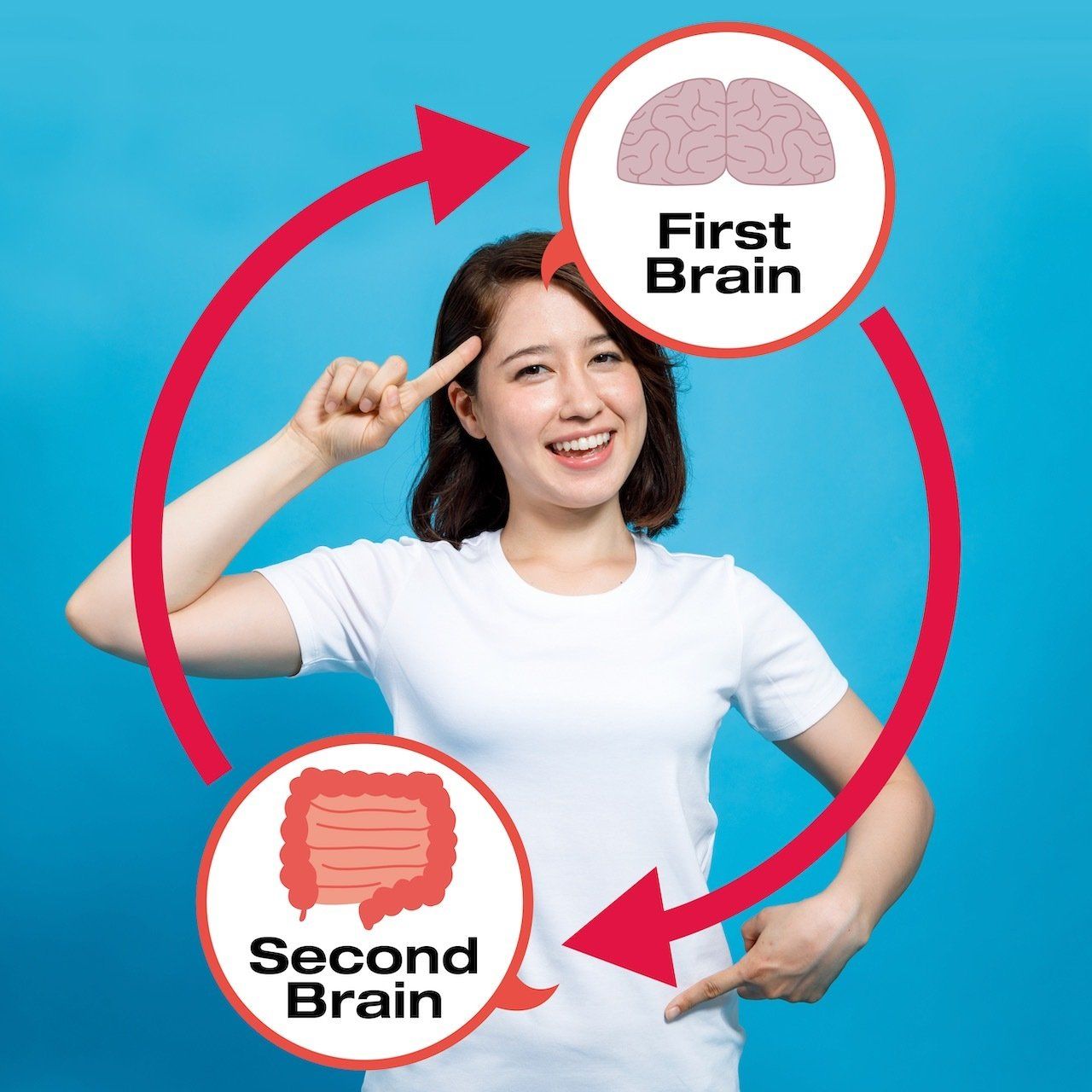
We often think of the prostate as a lone actor, measured by one number, PSA (prostate-specific antigen), and judged for enlargement or cancer risk. But biology doesn’t work in silos. The thyroid, a butterfly-shaped gland located in your neck, subtly influences how your prostate functions and how your PSA level is interpreted.
Understanding this connection can mean the difference between unnecessary worry and informed clarity.
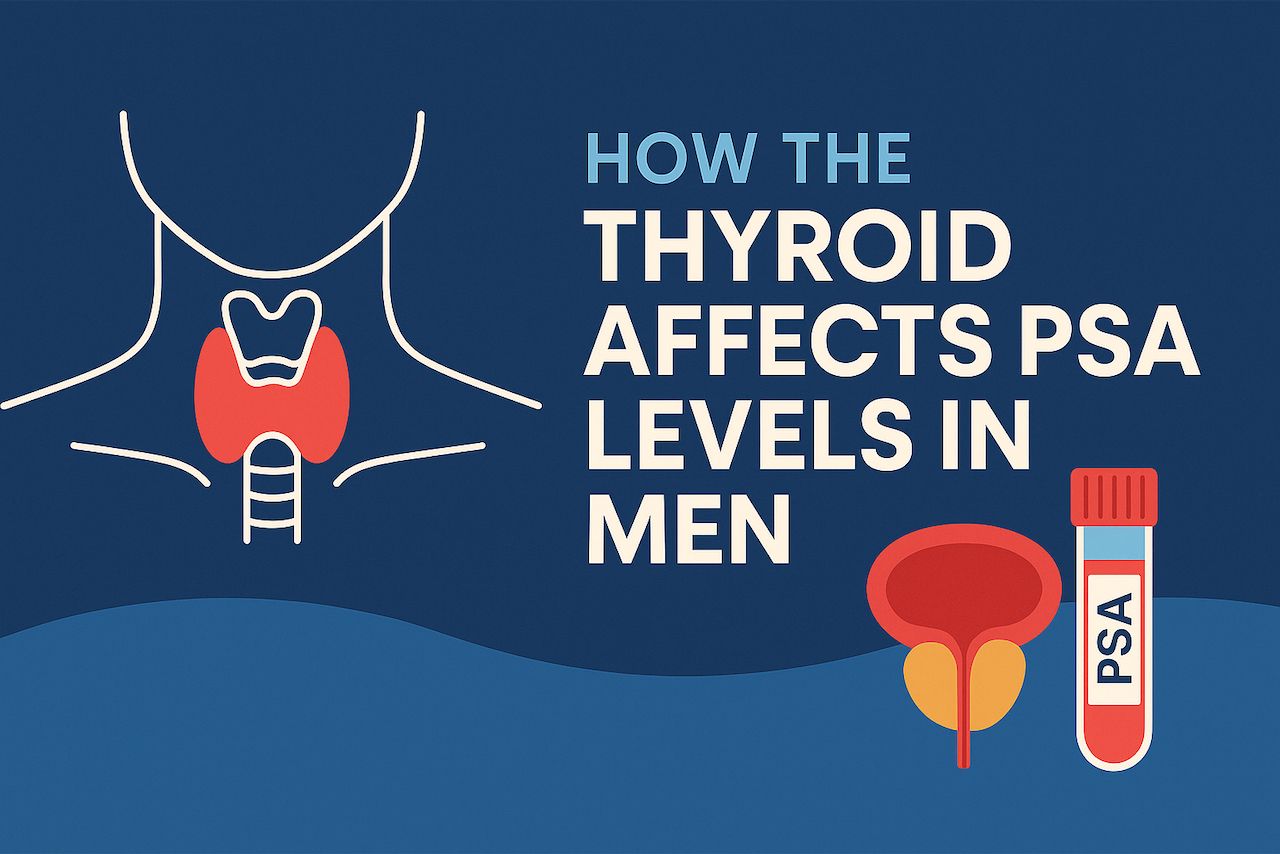
Why This Connection Matters
PSA is one of the most common markers doctors use to screen for prostate health. But it isn’t always straightforward. Thyroid imbalances, whether overactive or underactive, can influence PSA levels and create confusion.
In functional medicine, the question isn’t just what is happening, but why. Here, the “why” involves hormones, metabolism, and inflammation that link two glands you might not expect to see in the same conversation.
What the Science Says
Research shows thyroid status significantly affects PSA levels — sometimes inflating them, sometimes suppressing them, regardless of prostate cancer.
Science Spotlight: Thyroid Status and PSA
1. Hyperthyroidism (Overactive Thyroid)
- Mechanism: Excess thyroid hormone (T3/T4) increases metabolic activity and may stimulate androgen pathways, which can enhance prostate cell activity.
- Effect on PSA: Studies show men with hyperthyroidism often have elevated PSA levels, even without prostate cancer. This is thought to be due to increased prostate blood flow, gland stimulation, and possibly increased androgen receptor sensitivity.
2. Hypothyroidism (Underactive Thyroid)
- Mechanism: Low thyroid hormone tends to slow metabolism, lower testosterone levels, and reduce prostate stimulation.
- Effect on PSA: Hypothyroid men often show reduced PSA levels compared to euthyroid men. In some cases, PSA can rise again after thyroid hormone replacement.
This dual pattern explains why PSA cannot be interpreted in isolation. Thyroid status can raise or lower PSA — independent of malignancy.
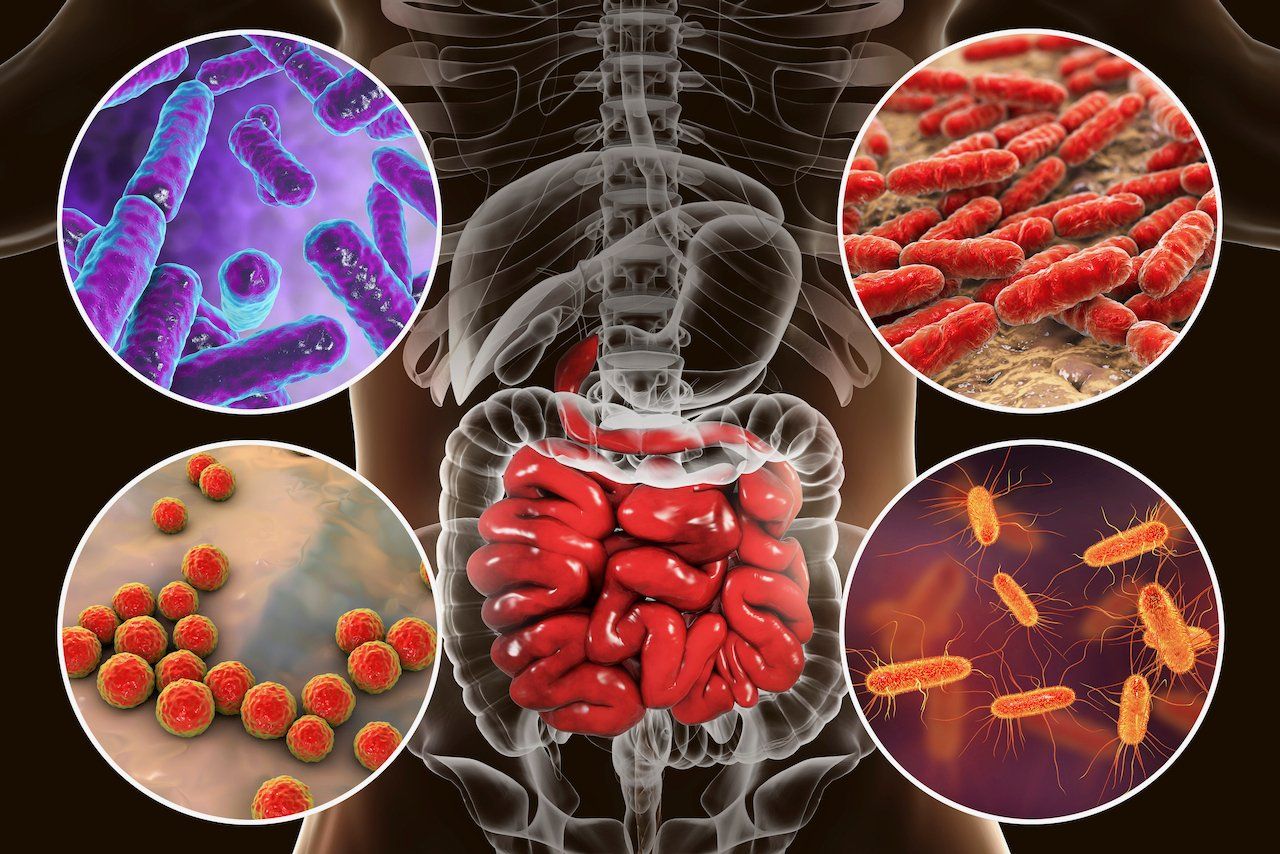
Functional Medicine Perspective: Looking Beyond TSH
In functional medicine, thyroid health is not a binary concept. It’s about how efficiently you produce, convert, and use thyroid hormones. Reverse T3, antibodies, and adrenal stress can all disrupt thyroid signaling and PSA levels.
Key Markers to Evaluate (Beyond Conventional Labs)
- TSH (Thyroid-Stimulating Hormone): First signal of thyroid stress, but misleading if looked at alone.
- Free T4 (Thyroxine): The storage hormone. Adequate T4 doesn’t guarantee it’s converting downstream.
- Free T3 (Triiodothyronine): The active hormone at the cellular level. Low free T3 levels indicate poor signaling, sometimes accompanied by normal T4 levels.
- Reverse T3 (rT3): A metabolic “brake pedal.” Elevated in stress, chronic illness, or inflammation, rT3 can block T3 at the receptor, leading to functional hypothyroidism even if blood levels look “normal.”
- Thyroid Antibodies (TPO, TgAb): Hashimoto’s autoimmunity alters long-term thyroid signaling and indirectly impacts PSA by affecting androgen balance and systemic inflammation.
- Sex Hormone–Binding Globulin (SHBG): Often elevated in hyperthyroid states, it lowers free testosterone and reshapes how the prostate responds.
- Cortisol & DHEA (Adrenal Crosstalk): Chronic stress raises rT3, lowers free T3, and indirectly suppresses androgen-driven prostate signaling.
Nutrition: Food as Endocrine Modulators
- Mediterranean Pattern: Olive oil, vegetables, legumes, fish. Reduces systemic inflammation (IL-6, CRP), stabilizes insulin, and balances thyroid–prostate signaling.
- Cruciferous Vegetables: Broccoli, kale, Brussels sprouts. Sulforaphane and indole-3-carbinol support estrogen metabolism and downregulate signals that promote prostate overgrowth.
- Pomegranate & Green Tea: Rich in polyphenols that suppress NF-κB and IGF-1 pathways, both linked to prostate inflammation and higher PSA.
- Omega-3 Fatty Acids: Improve cell membrane signaling, lower thyroid autoimmunity, and reduce prostate inflammation.
- Avoid Excessive Dairy & Red Meat: High intake is associated with elevated IGF-1 and higher PSA levels in some men.
Supplements: Precision Tools
- Vitamin D3 + K2: Supports immune regulation and has been shown to slow PSA rise in some men on surveillance.
- Zinc: Essential for thyroid hormone production and prostate integrity. Deficiency is linked with higher PSA and worse pathology.
- Selenium: Facilitates thyroid conversion (T4 → T3) and reduces oxidative stress in the prostate.
- Curcumin (Turmeric Extract): Potent NF-κB inhibitor. Studies have shown that it reduces prostate cell proliferation and inflammation.
- SSaw Palmetto + Pygeum: Reduce DHT activity, improve urinary flow, and often lower PSA in men with BPH.Ashwagandha & Adaptogens: Lower cortisol-driven rT3, improve thyroid balance, and stabilize PSA.
Lifestyle & Movement: Turning Down the Heat
- Exercise: 150+ minutes per week lowers PSA variability by reducing inflammation, balancing insulin, and optimizing testosterone metabolism.
- Weight Optimization: Central obesity drives insulin resistance and IGF-1, which stimulates PSA. Losing weight normalizes thyroid hormones and lowers PSA levels.
- Stress Reduction (Meditation, Breathwork, Prayer): Chronic stress raises rT3 and disrupts cortisol, destabilizing PSA.
- Sleep: Deep, restorative sleep helps raise melatonin, which in turn protects thyroid function and reduces the risk of prostate cancer.
Herbal & Botanical Allies
- Nettle Root: Reduces SHBG binding, moderates free testosterone activity, and helps lower PSA stimulation.
- Green Tea Extract (EGCG): Shown to slow PSA rise in men with prostate cancer and modulate thyroid autoimmunity.
- Resveratrol influences androgen receptor expression and lowers inflammatory markers associated with PSA elevation.
- Lycopene (Tomatoes, Watermelon): Antioxidant with specific data for prostate health; higher intake correlates with lower PSA.
Genomics Meets Lifestyle
Certain genetic variants influence how nutrition, stress, and hormones play out in the thyroid–prostate axis:
- MTHFR (methylation): Poor methylators benefit from methylated B vitamins to optimize thyroid conversion and reduce inflammatory PSA drivers.
- TCF7L2 (insulin resistance): Maintaining blood sugar balance via Mediterranean eating is non-negotiable for prostate and thyroid health.
- FOXO3 (longevity): Modulates stress resistance; lifestyle practices, such as fasting and exercise, upregulate FOXO3, thereby reducing PSA-promoting inflammation.
Integration Point: Genetics + thyroid function + lifestyle = personalized prostate strategy.
Putting It All Together
- Hyperthyroid → PSA goes up.
- Hypothyroid → PSA goes down.
- Normalizing thyroid function → normalizes PSA.
- Nutrition, supplements, herbs, exercise, stress mastery, and sleep → tools to keep both thyroid and prostate balanced.
PSA doesn’t just measure the prostate. It reflects the orchestra of thyroid hormones, metabolism, and lifestyle signals that shape a man’s biology.
Your health isn’t random. It’s written in code. Every cell in your body carries a script. Your genes don’t just predict your future—they respond to what you eat, how you move, and the choices you make daily. That’s the journey I share in “Understanding Genomics: How Nutrition, Supplements, and Lifestyle Can Help You Unlock Your Genetic Superpowers”.
Read the code. Live the design. The rest follows.
Dr. Marios Michael
Medical Disclaimer: The information included on this blog is for educational purposes only. It is not intended nor implied to be a substitute for professional medical advice. The reader should always consult his or her healthcare provider to determine the appropriateness of the information for their own situation or if they have any questions regarding a medical condition or treatment plan. Never disregard professional medical advice or delay in seeking it because of something you have read on this blog! Reading the information on this blog does not create a physician-patient relationship.
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.